Services
Our Services
Rapheephan Clinic provide comprehensive and collaborative care to women of all ages, from family planning, to midwifery and delivery care, mid-life healthcare, menopause and post-menopause counseling and management, prevention of such diseases such as cervical cancer , menopause, and diagnosis of both cancerous and non-cancerous tumors.
01.
Prenatal Care and Delivery
02.
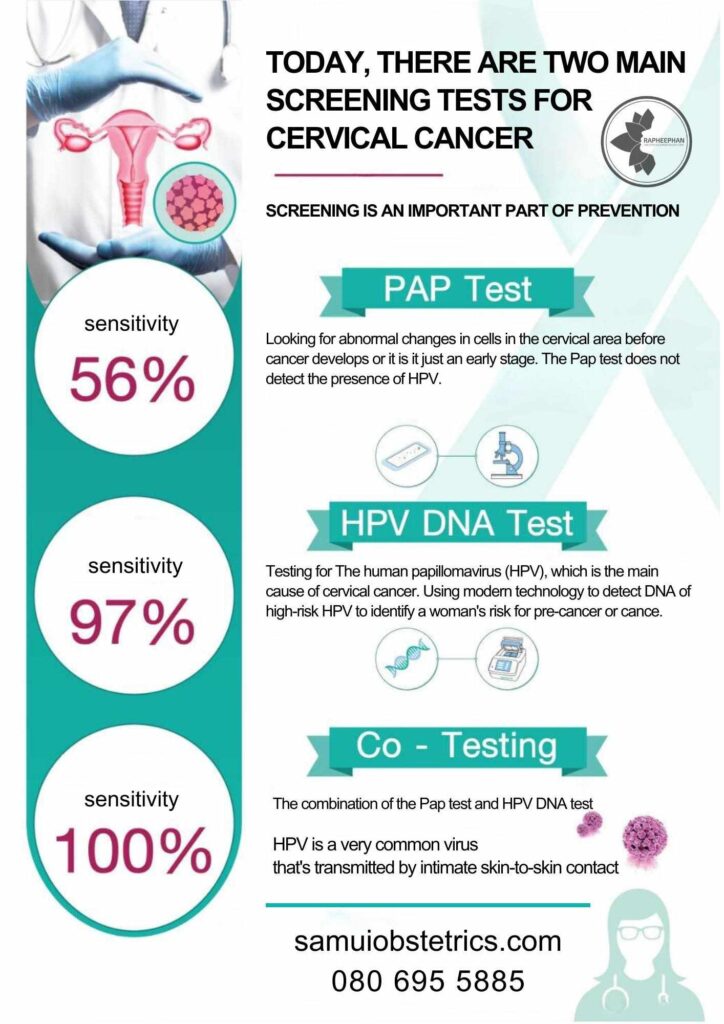
PAP Test and
HPV Test
03.
Colposcopy
04.
Contraceptive Management
05.
STD Test
06.
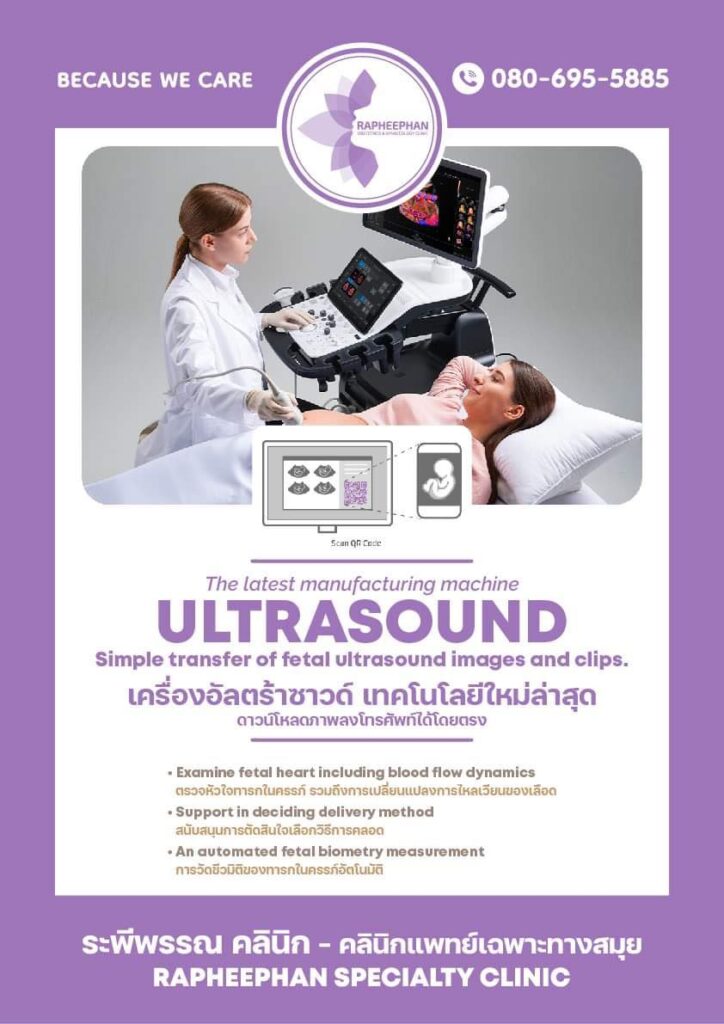
Obstetrics
Ultrasound 2D
07.
Ultrasound
Abdomen
08.
Women's Health
Check Up
09.
Cosmetic Gynecoloty
10.
Male Vasectomy
11.
Circumcision
12.
Prostate biopsy
Hysterectomy
A Hysterectomy is a surgical removal of the uterus. It ends menstruation and the ability to become pregnant.
Why is it done?
Hysterectomy may be performed to treat:
- Abnormal uterine bleeding that is not controlled by other treatment methods
- Severe endometriosis (uterine tissue that grows outside the uterus)
- Uterine fibroids (benign tumors) that have increased in size, are painful or cause bleeding
- Increased pelvic pain related to the uterus but not controlled by other treatment
- Uterine prolapse – (uterus that has “dropped” into the vaginal canal due to weakened support muscles) that can lead to urinary incontinence or difficulty with bowel movements
- Cervical or uterine cancer
- Complications during childbirth (like uncontrollable bleeding)
Types Of Hysterectomies
There are four types of hysterectomies in which can be performed depending on the condition and severity of the patient. These four types are:
- Vaginal hysterectomy
- Laparoscopic hysterectomy
- Minilaparotomy (a “short incision”) hysterectomy
- Abdominal hysterectomy
These procedures are listed in order of preference, ranked by criteria such as scarring and recovery time.
Koh Samui Hospital provide abdominal hysterectomy and vaginal hysterectomy(for prolapse uterus)
Vaginal Hysterectomy
With this procedure, the doctor accesses the uterus through the vagina. A vaginal hysterectomy and is often preferred by patients because:
- It does not leave any visible scars: the internal sutures are the same as the other procedures, but because the access point is different, there are no scars or open wounds on the skin.
- There is a significant reduction in the time it takes to become active after the surgery.
- Lower complication rate:
- There is less of a chance of any infection to the surgical site.
- There is far less of a chance of causing damage to any other organ.
In the past, vaginal hysterectomies were only used when the conditions were optimal for the procedure. Now, as the skill of our surgeons has grown, vaginal hysterectomies can be used even under complicated conditions. It is important to note that it is possible to have this procedure if you have had a Caesarean section.
This procedure must be done by a surgeon specifically trained in the vaginal hysterectomy method.
Abdominal Hysterectomy
Abdominal hysterectomies are usually performed only when needed. These types of operations typically require a 15 cm incision to perform. While an abdominal hysterectomy is quite safe to perform, it has a longer recovery time and more risk of scarring. Hence in more advanced hospitals, and in conditions which allow it, other types of hysterectomies are performed.
General Information on Hysterectomies
A hysterectomy generally takes 1 to 3 hours. It may be performed under general or regional anesthesia. During a Hysterectomy, the uterus may be completely or partially removed. The fallopian tubes may also be removed. After surgery, a catheter may remain in place for 1 to 2 days to help the bladder pass urine. The average hospital stay depends on the type of surgery, but is usually 1 to 3 days.
Risks & complications
There are possible risks and complications associated with anesthesia, including respiratory or cardiac malfunction. Other complications include:
- Wound complication (i.e. abscess, disruption)
- Excessive bleeding or blood clots
- Infection
- Bladder, ureter or bowel injury
- Pain with intercourse, decreased libido, or reduced ability to have an orgasm
- Temporary abdominal distention due to bowel ileus or transient decreased bowel movement
Following surgery, some women may feel a sense of loss or become depressed, but these emotional reactions are usually short-lived.
Risks can be reduced by following the surgeon’s instructions before and after surgery.
Alternatives
Alternate treatment options will depend very much on the source of the problem. The surgeon may discuss alternative approaches to Hysterectomy:
- Birth control pills or other medications may be helpful in treating prolonged bleeding
- Endometrial ablation (removal of the lining of the uterus) may help with very heavy periods
- Drugs can be used to shrink uterine fibroids
- Myomectomy, or surgical removal of fibroids, is major surgery; one in three women have tumors recur in 5 years
- Chronic pain may be treated with anti-inflammatory drugs, birth control pills, or physical therapy Expectations after Surgery
Removal of the ovaries along with the uterus in premenopausal women causes immediate menopause, and estrogen replacement therapy may be recommended.
Baby Delivery
Deciding on the place for your baby to first see the world is an important decision for a mother and father. Koh Samui hospital has modern delivery rooms, offering up-to-date equipment and technology, in a safe, and warm environment.
Baby Delivery Options
Koh Samui’s delivery rooms are available 24 hours a day with the following services:
- Natural childbirth: This is a preferred option for a healthy mother and a baby with no abnormalities, as there are no risks of surgical complications and infection. Childbirth through the birth canal drains the amniotic fluid from the baby’s lung, enabling enlargement of the lung in a natural process.
- Vaginal childbirth with epidural analgesia: Another option for healthy mothers and babies, with this version of natural childbirth our doctors use a spinal block to reduce the pain of the delivery by injecting medication into the spinal column. Even though the pain is reduced, there is still the feeling of your baby passing through the birth canal.
- Cesarean section: This is the safest ways to give birth if a mother cannot do so naturally, due to a mother’s medical condition, a problem with the baby or the baby’s position in the womb. As a C-section is a surgical procedure, there is greater blood loss and a longer recovery time due to the need to care for an incision point. Healthy mothers and babies can also safely have Cesarean sections, but the mother should understand the after delivery care issues.
At the time of delivery, a medical team consisting of your doctor, anesthesiologists, nurses and your doula will closely provide care for the mother and baby. As soon as the baby is born, the nursery staff will take diligent care of your baby’s health.
Should there be the slightest abnormality detected, the baby will be placed under the prompt care of our ICU physicians and specialty trained nurses available 24 hours a day, 7 days a week.
We have specific services to help with any complications which may arise with you or your baby. We can monitor the health of the two of you at all stages of the pregnancy, especially with any of the following concerns:
- If the mother has a history of difficult childbirth, miscarriage or surgery of the uterus
- If the mother has a history of preterm delivery (before 37 weeks)
- If there are complications such as diabetes, hypertension, kidney disease, heart disease, etc.
- Mothers younger than 16, or older than 40 years old
- Pregnancy with twins
- The fetus is in the breech position, or has a positioning issue (identified at 34 weeks and onwards)
- The size of the uterus does not correlate with the gestational age
- If the baby weights less than 2,500 grams, or more than 4,000 grams
- If bleeding occurs during the pregnancy
- If the mother is greater than 40 weeks pregnant
- If the baby’s growth is less than 1 kg/month after the 24th week
- Heart NST (Non Stress Test): After the baby is moving in the womb, a Heart NST can be performed to check the baby’s heart if the mother has any of the following conditions: ◦Diabetes, hypertension, heart disease and other similar complications
- Irregular movement of the baby
- Overdue pregnancy
- The volume of amniotic fluid is above or below normal, which can cause birth abnormalities
- The fetus is growing more slowly than usual
Pap Test (Pap Smear)
The pap test or pap smear is performed to detect cervical cancer. A doctor will insert a speculum into the vagina to widen it and cells from the cervix will be collected for analysis in the laboratory. Abnormal or mutated cells may cause or indicate cervical cancer.
Who Should Undergo a Pap Smear?
We recommend discussing with your doctor the best time for you to undergo the pap smear and how often. The American Cancer Society has issued the following recommendations for women regarding the pap smear:
- All women over 21 years of age or within three years for the first sexual intercourse should undergo a Pap Smear, depending on whichever time arrives first. The test should be repeated every one to two years after that.
- Women over 30 years of age should undergo an annual Pap Test. After three consecutive normal Pap Smear results, these women may undergo the test every three years, with the exception of those at risk for cervical cancer, such as women infected by HIV or HPV (human papillomavirus), those with compromised immune systems, or women who used diethylstilbestrol during pregnancy. Women at risk for cervical cancer should continue annual Pap Tests.
- Women over 70 years of age who have had normal results for three consecutive years and no abnormal results in the last ten years and who are not at risk for cervical cancer do not need to undergo any more Pap Tests.
Preparing For a Pap Smear
- A Pap Test should be performed when you are not menstruating.
- Do not douche before the test.
- Do not use any vaginal suppositories, creams, or spermicide 48 hours before the test.
- Do not have sexual intercourse at least 24 hours before the test.
Cosmetic Gynecology